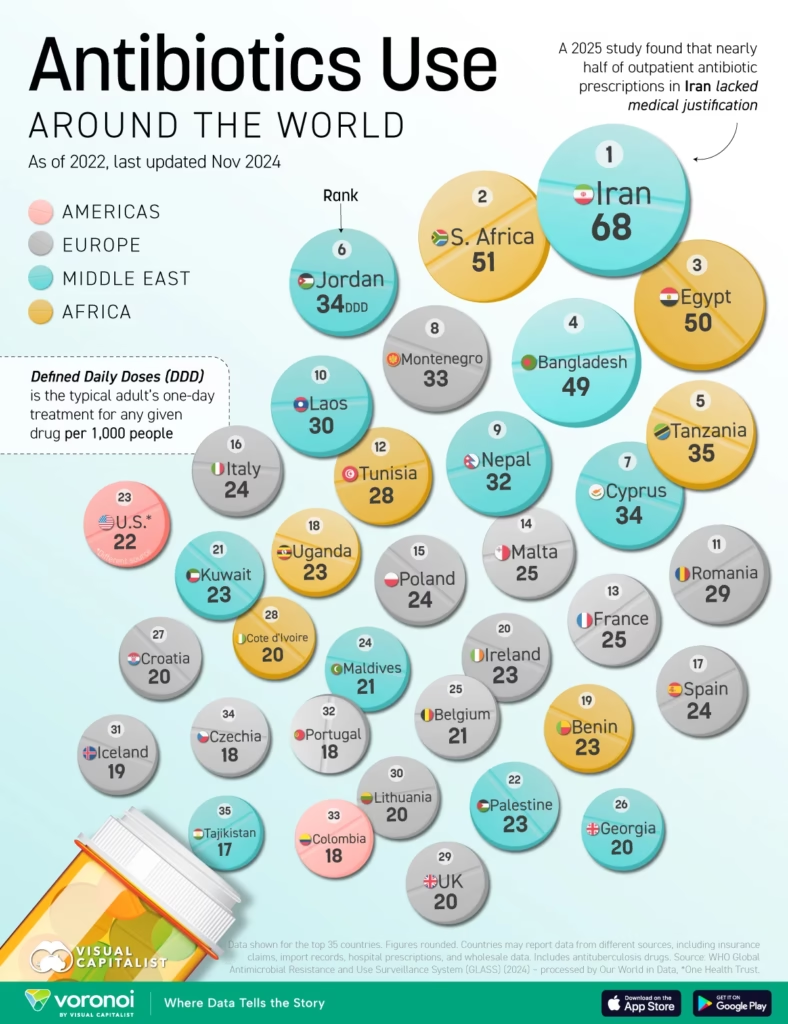
Are antibiotics being prescribed more often than necessary

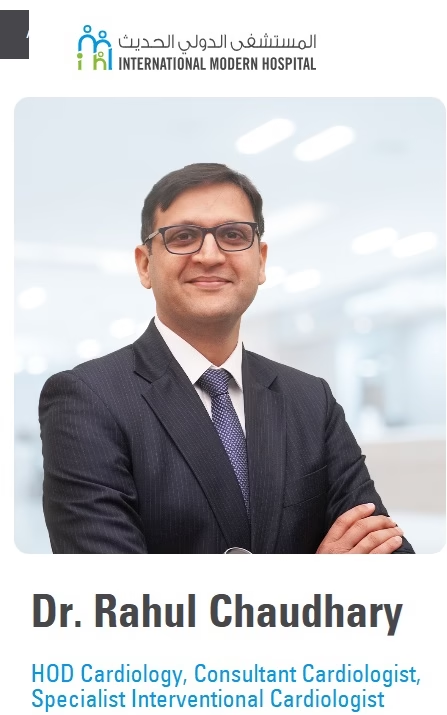
Dr Rania Alkhani, Pharmacy Manager at International Modern Hospital Dubai
1. From your experience, are antibiotics being prescribed more often than necessary in the UAE or elsewhere?
Antibiotics are among the most commonly overused and misused medications, both in the UAE and globally. In the past, it was common for people to take antibiotics for almost any sign of infection. However, medical advances have clearly shown that not all infections are caused by bacteria. In fact, many common illnesses—especially upper respiratory infections such as colds and flu—are viral, and antibiotics provide no benefit in these cases.
Using antibiotics when they are not needed exposes patients to unnecessary side effects and, more importantly, increases the risk of antibiotic resistance. This misuse allows bacteria to adapt and become resistant, leading to the emergence of so-called “superbugs” that are much harder to treat in the future.
Even when an infection is bacterial, antibiotics are not a one-size-fits-all solution. Different bacteria respond to different antibiotics, and treatment should be targeted whenever possible. The goal is to use the most appropriate, narrow-spectrum antibiotic to effectively treat the infection while minimizing the risk of resistance.
Simply put, antibiotics should be used wisely—because it is not always necessary to use a gun to kill a fly.
2. Do you find that some expats bring antibiotics from their home countries — and in what situations do you most often see misuse?
Yes, this does happen quite frequently. Some expats and visitors bring medications from their home countries, including antibiotics, for several reasons. In some countries, generic medicines are more affordable, and in others antibiotics may be available without a prescription. In the UAE, antibiotics are strictly regulated and cannot be dispensed without a valid prescription, as part of national efforts to control misuse and resistance.
Because of these differences, some people prefer to bring antibiotics with them so they have them readily available when they feel unwell.
The most common misuse we see is taking antibiotics for viral infections, such as colds, flu, or sore throats, where antibiotics are ineffective. Another serious form of misuse is stopping antibiotics as soon as symptoms improve—often after one or two days—rather than completing the full prescribed course. This practice increases the risk that bacteria survive, become resistant, and cause more difficult-to-treat infections in the future.
3. When antibiotics are overused or taken incorrectly — for example, for viral illnesses — what are the real risks for patients and the wider community?
Our bodies naturally contain millions of bacteria that live with us and help protect our health. When antibiotics are used unnecessarily—such as for viral illnesses—or taken incorrectly, they do not only kill harmful bacteria, but also destroy the beneficial bacteria that keep this balance. This disruption allows more harmful bacteria to grow and spread.
Over time, repeated or inappropriate use of antibiotics encourages bacteria to become resistant. These resistant bacteria, often referred to as “superbugs,” are much harder to treat and may require stronger, more toxic, or more expensive medications. In some cases, treatment options become very limited.
For the wider community, antibiotic resistance is a serious public health threat. Resistant bacteria can spread between people, making common infections more difficult to control and increasing hospital stays, complications, and healthcare costs. Overuse of antibiotics in the past has already reduced the effectiveness of some of our strongest, broad-spectrum antibiotics, and this makes treating serious infections increasingly challenging.
Using antibiotics responsibly protects not only the individual patient, but also the safety and health of the entire community.
4. What steps are hospitals, clinics, and patients already taking — or should be taking — to reduce unnecessary antibiotic use?
Healthcare facilities already play an important role in reducing unnecessary antibiotic use, and this effort needs to continue and strengthen. Antibiotics should remain restricted medications and only be prescribed by qualified healthcare professionals when there is a clear medical indication.
In hospitals and clinics, this means confirming bacterial infections whenever possible before prescribing antibiotics. Simple and appropriate tests—such as urine tests for suspected urinary tract infections, stool tests when indicated, respiratory panels for certain respiratory symptoms, and relevant blood tests—help clinicians identify the cause of infection and choose the most suitable treatment. This ensures that antibiotics are used only when needed and that the right antibiotic is selected.
Patients also have an essential role. Public awareness is key to reducing misuse. Patients should avoid requesting antibiotics for colds or flu, follow medical advice, and always complete the full course when antibiotics are prescribed.
Responsible prescribing by healthcare providers, combined with informed and cooperative patients, is the most effective way to protect the effectiveness of antibiotics for future generations.

 English
English